New formation of neurons from stem cell niche disrupted after stroke
Freiburg, 24.10.2024
Researchers at the University of Freiburg have studied what happens immediately after a stroke in the stem cell niche known as the subventricular zone, using a mouse model. This revealed a mechanism that results in fewer newborn neurons from the stem cell niche surviving after stroke, thereby significantly limiting the neurogenic reaction of the subventricular zone to repair the brain. This fundamental understanding of the cellular processes in the brain could help in future to boost the body’s own repair to replace lost neurons and ameliorate the consequences of stroke.
In healthy rodent brains, newborn neurons are constantly generated in the stem cell niche, known as the subventricular zone (SVZ). These cells might help to repair a brain that has been damaged by disorders of the central nervous system. After brain damage, the SVZ responds by forming newborn neurons that migrate towards the area of the lesion and could provide cell replacement there. However, after a stroke, the functioning of the body’s own repair system, the neurogenic response by the SVZ, is very limited. Researchers headed by Prof. Dr. Christian Schachtrup, professor at the Institute of Anatomy and Cell Biology at the University of Freiburg, and his former doctoral student Dr. Suvra Nath, have studied the mechanisms underlying this limited response to repair the brain.
Stroke negatively influences interaction of microglia and neurons
The vasculature, that is, the system of blood vessels of the SVZ, becomes more permeable after a stroke. As a result, the protein fibrinogen and others reach the stem cell niche, and this in turn influences the local microglia cells. These central nervous system immune cells are immediately activated by the changes in the stem cell niche, affecting the cell cycle progression of the neural stem cells leading to cell death of newborn neurons. “The SVZ stem cell niche is a fragile system. Microglia, the defence cells of the brain, are an integral component of the characteristic SVZ microenvironment and govern the behaviour of the neural stem cells. These interactions in the stem cell niche are disrupted after a stroke,” explains Schachtrup.
A check test also suggests that the interactions between activated microglia and neural stem cells in the SVZ negatively influence the neurogenic repair: restoring the original SVZ microenvironment increases the neurogenic repair – even after stroke. At the same time, more newborn neurons survive in the SVZ if the activated microglia cells are reduced.
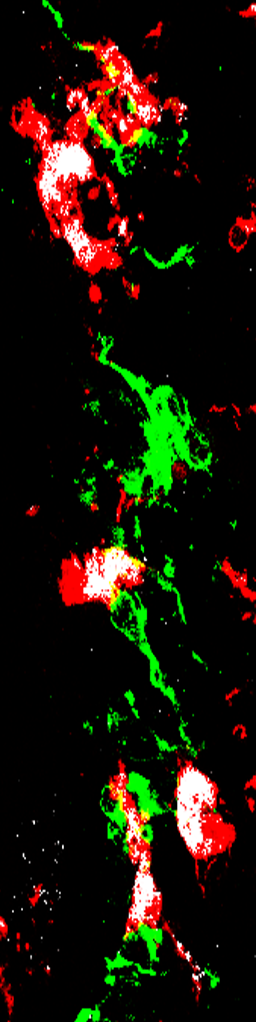
SVZ stem cell niche after stroke: After a stroke, the altered stem cell niche environment leads to a rapid activation of microglia (grey) and their altered interaction with neural stem cells (green). This leads to cell death of the newly formed neurones in the stem cell niche and a greatly reduced endogenous repair process for the stroke region.
“A better understanding of the cellular processes is bringing us closer to being able to promote the body’s own repair of the brain.”
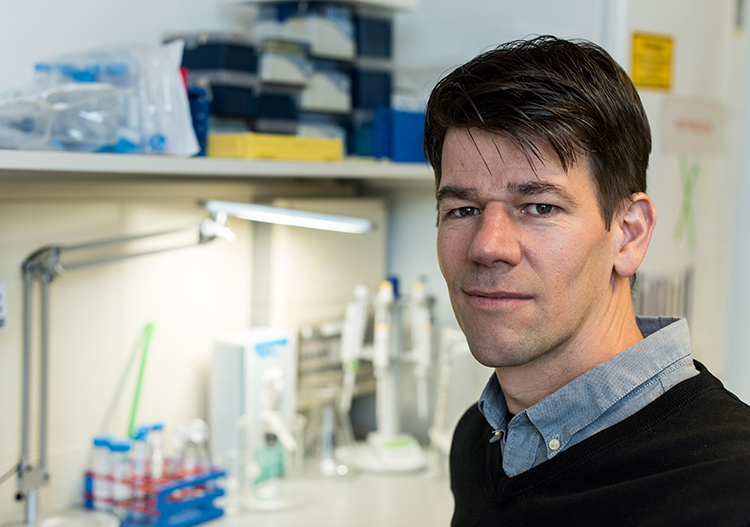
Prof. Dr. Christian Schachtrup
Professor at the Institute of Anatomy and Cell Biology at the University of Freiburg
Ameliorating the consequences of stroke
The processes described by the researchers begin very shortly after a stroke. In order to understand them, they had to rely on mouse models. Although the human brain also has an SVZ, new neurons are only produced in the first year of life and this cell production is dormant after that. The researchers believe it is possible that this production could be reforced by medical intervention. “When we understand the mechanisms of how the neural stem cells are differentiating and how extracellular factors influence the development of newborn neurons, this will bring us closer to promote the endogenous repair of the brain in central nervous system disorders,” says Schachtrup. Next, the researchers want to study interactions between microglia cells and neural stem cells in human organoids. This method is bringing them closer to the goal of understanding similar processes in the human brain.
Facts overview
- Original publication: Nath et al., Interaction between subventricular zone microglia and neural stem cells impacts the neurogenic response in a mouse model of cortical ischemic stroke. Nature Communications. DOI: 10.1038/s41467-024-53217-1
- The authors Dr. Suvra Nath, Jose Carlos Martínez Santamaría, Dr. Yu-Hsuan Chu, Dr. Pasquale Conforti, Dr. Jia-Di Lin, Kexin Wu and Dr. Sachin S. Deshpande research at the Medical Faculty’s Institute of Anatomy and Cell Biology at the University of Freiburg and the Faculty of Biology. Dr. Roman Sankowski and Dr. Lukas Amann are researchers at the Institute of Neuropathology of the Medical Faculty. Prof. Dr. Andreas Vlachos is Professor of Neuroanatomy at the Medical Faculty as well as at the BrainLinks-BrainTools center and at the Center for Basics in NeuroModulation (NeuroModulBasics). Prof. Dr. Marco Prinz is Professor of Neuropathology at the Medical Faculty, at the Centre for Biological Signalling Studies (BIOSS) and at the Centre for Integrative Biological Signalling Studies (CIBSS) Cluster of Excellence at the University of Freiburg as well as at the Center for Basics in NeuroModulation (NeuroModulBasics). James S. Choi and Prof. Dr. Jae K. Lee from the University of Miami also make up the team of authors.
- The study is funded by the German Research Foundation (SFB/TRR167, SCHA 1442/8‐1, SCHA 1442/8‐3, und SCHA 1442/9‐1).